 Posted By Akio
Posted By Akio- Comments 0
Retinal Detachment Symptoms, Signs, Causes, and Treatment
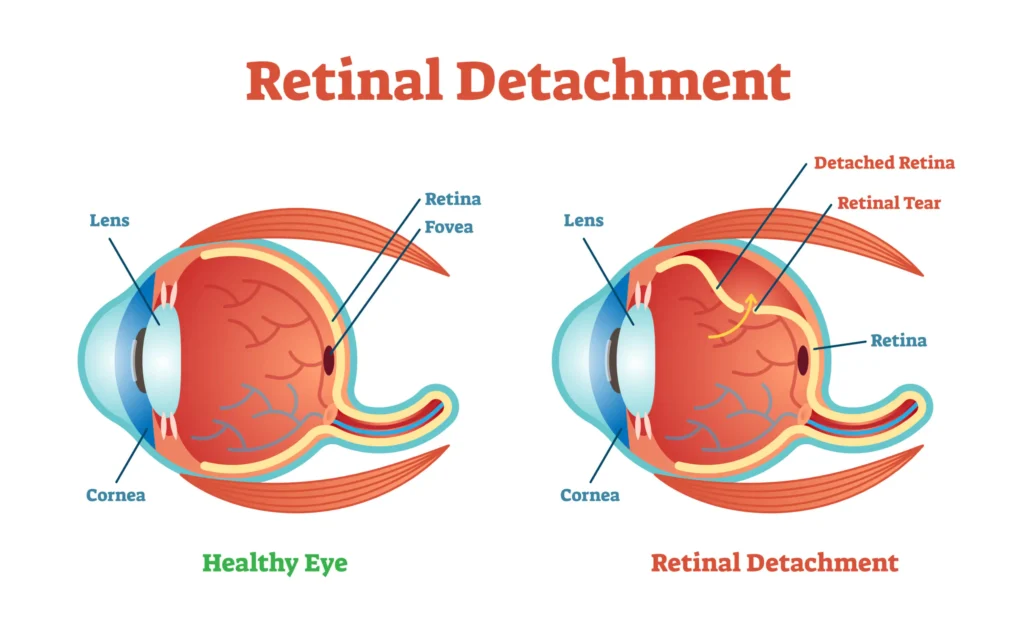
The retina is a thin layer of tissue located near the optic nerve. It captures incoming photons and transmits them to help the brain perceive a visual image. Retinal detachment occurs when the retina is detached from its usual position. Although painless, this condition hurts vision and may lead to blindness.
In this blog, we will talk about the symptoms, signs, causes as well as treatment options for Retinal detachment.
Retinal Detachment Causes: Who Is at Risk?
Although Retinal detachment is a common condition that occurs in almost everyone, some factors may increase your risk of developing this condition, such as:
- Having undergone a serious eye injury.
- Being extremely near-sighted, like having a high myopia.
- Having a family history of retinal detachment.
- Previous retinal detachment in one eye.
- Having undergone a Posterior vitreous detachment.
- Having a weak retina, that is, a history of holes in the retina.
Types of Retinal Detachment & Their Causes
Based on the state of your retina, there are multiple types of retinal detachment. Each type happens due to a different cause that leads to the detachment, such as:
Rhegmatogenous Retinal Detachment
Rhegmatogenous retinal detachment is the one that occurs most commonly, as it is caused due to ageing. Rhegmatogenous detachments are caused when there’s a tear in your retina which allows the gel-like fluids known as Vitreous Humor from your eye to collect behind the retina. This fluid pushes the retina away, leading to its detachment.
Other factors that can increase your risk for this type of retinal detachment are having eye injuries, near-sightedness, and eye surgery.
Tractional Retinal Detachment
Tractional retinal detachment commonly occurs due to diabetic retinopathy, which is an eye condition among diabetic people. This is because high blood sugar levels can damage blood vessels in the retina and cause scar tissue which gets bigger and can pull on your retina, detaching it in the process.
Thus, not only is it essential for a diabetic person to get a comprehensive dilated eye exam once a year, but it is also vital to manage your diabetes by staying physically active and developing healthy eating habits.
Other factors that can increase your risk for tractional retinal detachment are eye diseases, eye infections, and swelling.
Exudative Retinal Detachment
Exudative retinal detachment commonly occurs when the fluid builds up and gets trapped in the back of your eye, causing the retina to detach. Unlike others, this type of retinal detachment doesn’t involve a retinal tear. It commonly occurs due to retinal diseases like Coats disease, retinal cancer, AMD, eye tumours, uveitis, etc.
Retinal Detachment Symptoms: How to Identify Early Signs
Retinal detachment may not show any symptoms if only a small part of the retina is detached. However, if the macula is detached, you may notice symptoms like:
- Emergence of a shower of floaters across your vision
- Photopsia: A Large number of flashes of light in your eyes
- Darkening of your peripheral vision
- A curtain-like formation over your field of vision
- Inability to see/Vision getting impaired
How is Retinal Detachment Diagnosed?
To diagnose retinal detachment, you need to give a dilated eye exam to get your retina checked. This is done by putting in eye drops which help dilate the pupil of your eye. Retinal detachment is usually diagnosed through painless and non-invasive methods such as:
Optical Coherence Tomography
In this test, you’ll get dilating eye drops and will be asked to sit in front of the OCT machine which will scan your eye.
Fundus imaging
In this test, wide-angle images of your retina are taken after your eyes are dilated
Ocular ultrasound
In this test, your eyes are scanned using an instrument. Then gel is applied on your eyelids and scanned again with eyes closed. This test doesn’t require dilating eye drops, but your eyes are usually numbed to avoid discomfort.
Computed Tomography
Also known as a CT scan, this test uses X-rays to identify any eye injuries or trauma to ensure safe treatment.
Retinal Detachment Treatment Options: What Works Best?
Surgery is often advised to repair a retinal tear or detachment. Depending on the risks and benefits of each treatment option available, you can determine which treatment option will suit you the best. Some of these treatments are:
- Photocoagulation
Also known as laser surgery, this procedure involves using a laser beam to burn through the retinal tear, creating a scar that connects the retina to the underlying tissue and holds it in place.
- Cryopexy
Also known as freezing, this procedure involves putting a freezing probe on the surface of the eye which causes a scar that helps keep the retina intact.
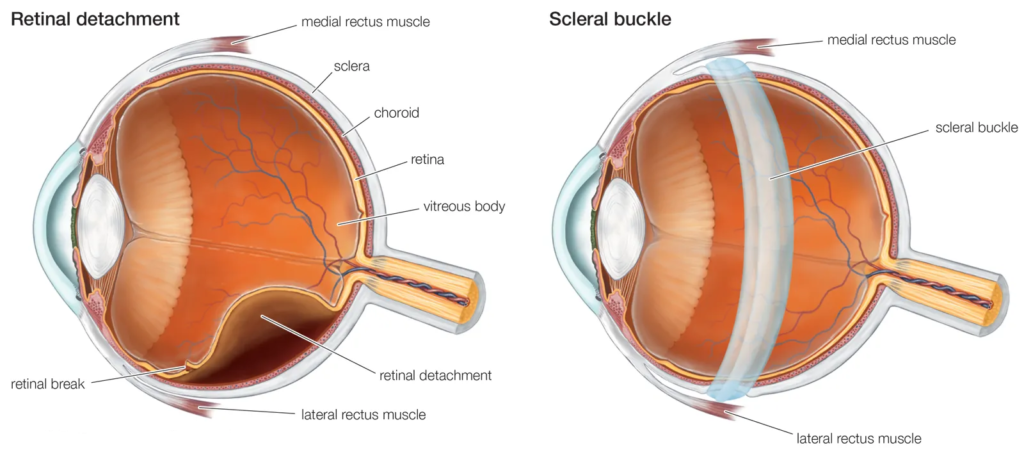
- Scleral buckling
This surgery involves sealing the retinal tear by placing a silicone band around the eye to hold the retina in place and sealing the tear with a laser.
- Vitrectomy
This surgery helps remove the vitreous by using the laser to seal all retinal tears and placing a bubble of gas, oil, or air to help the retina stay intact.
- Pneumatic retinopexy
This procedure is used in minor detachments. It involves inserting some fluid in the eye with the help of a needle, injecting a small air bubble into the eye, and then waiting for the retina to move back into place as you repair any tears with the help of Photocoagulation or Cryopexy.
Recovery After Retinal Detachment Surgery: Essential Tips
It is often advised to follow some tips to ensure recovery after retinal detachment surgery, such as:
- Taking enough rest
- Not picking up heavy weights/avoiding jerks
- Maintaining the position as advised by the Ophthalmologist
- Avoiding altitude change
- Keeping activity levels low
- Wearing an eye patch till the recommended time
Sleeping Position & Post-Surgery Do’s and Don’ts
After a retinal detachment surgery, it is crucial to follow post-surgery guidelines to ensure proper healing of your eye. The following tips may be recommended:
- Keeping your head tilted to the opposite side of the retinal tear to allow the gas bubble to stay in its place.
- Sleeping with your face down by keeping pillows on the side for one night after the surgery to prevent you from rolling in a different position.
- If your ophthalmologist allows you to lay on your side, it is important to keep pressure off the operated eye by sleeping on the opposite side of the operated eye.
- Following the instructions of sleeping post-surgery as advised by your Ophthalmologist, as every RD is different from one another.
Conclusion: Why Early Diagnosis & Treatment Are Crucial
Treatment for retinal detachment works well if the detachment is detected early, to prevent vision loss. If you experience any sudden changes in your vision, flashes of light, or a curtain-like shadow in your vision, it is recommended to take a dilated eye exam with an ophthalmologist immediately. With prompt diagnosis and treatment, retinal detachment can be successfully repaired, allowing you to preserve your vision.
At the AK Institute of Ophthalmology, we perform 3D Retina surgery for Retinal detachment (RD). For the best results of Retina Detachment surgery, and on facing any of the above symptoms, kindly visit AKIO.
Visit AKIO, the trusted Cataract Treatment in Delhi NCR, for advanced treatments and personalized care. Book your appointment today!”



